Every BPC-157 Human Trial Up to 2026: What the Research Actually Shows
Summary
BPC-157 has generated massive interest in the peptide community for its healing potential. But here’s the uncomfortable truth: despite decades of promising animal research, human clinical data remains extremely limited.
The Current State of Human Evidence
- Only 3 published human studies exist as of early 2026—all pilot studies with small sample sizes
- The largest trial was cancelled: A 2015 Phase I study with 42 volunteers never published results
- Total human subjects studied: Fewer than 30 people across all published trials
- No randomized controlled trials: All existing studies lack placebo controls
What the Human Studies Show
- Interstitial cystitis (2024): 12 patients, 80-100% symptom resolution with bladder injections
- Knee pain (2021): 16 patients, 87.5% reported significant relief at 6-12 months
- IV safety (2025): 2 adults tolerated up to 20mg IV with no adverse effects
Regulatory Reality
- FDA Category 2 (2023): Cannot be legally compounded due to insufficient safety data
- WADA prohibited (2022): Banned under S0 Unapproved Substances for all athletes
- Not approved anywhere: No regulatory agency worldwide has approved BPC-157 for human use
The Gap Between Animal and Human Research
If you’ve read about BPC-157 online, you’ve likely encountered impressive claims: accelerated tendon healing, gut repair, nerve regeneration, and more. These claims come from a substantial body of animal research—over 100 studies spanning three decades.
The problem? Almost none of this has been validated in humans.
A 2025 systematic review in the American Journal of Sports Medicine examined all BPC-157 research for orthopaedic applications. Of 544 articles screened, only 1 clinical study met inclusion criteria. The other 35 included studies were preclinical animal models.
“Despite its growing popularity among athletes and its wide availability through non-regulated sources, there is minimal human data available.” — Vasireddi et al., American Journal of Sports Medicine, 2025
This gap matters. Animal studies don’t always translate to humans. Mice and rats have different metabolisms, healing responses, and drug sensitivities. What works remarkably well in a rodent may not work—or may even be harmful—in people.
The Cancelled Phase I Trial
The most significant missed opportunity in BPC-157 research occurred in 2015-2016.
What Was Planned
PharmaCotherapia sponsored a Phase I clinical trial (NCT02637284) designed to be the first rigorous human safety study of BPC-157. The study enrolled 42 healthy volunteers aged 18-35 and aimed to establish:
- Safety profile in humans
- Pharmacokinetic data (how the body processes BPC-157)
- Optimal dosing parameters
What Happened
In 2016, the researchers cancelled submission of results. No data was ever published. No explanation was provided publicly.
This leaves a critical gap: we still don’t have the foundational pharmacokinetic data that would normally inform human dosing. The doses people use today are essentially extrapolated from animal studies—not based on actual human metabolism data.
The Three Published Human Studies
As of December 2025, only three human studies on BPC-157 have been published. All were conducted by the same research group in Florida, and all are small pilot studies without placebo controls.
1. Intraarticular Knee Injection Study (2021)
Study design: Retrospective review Participants: 16 patients with chronic knee pain Intervention: Intraarticular injection of BPC-157 (2cc of 2000 mcg/mL solution) Follow-up: 6-12 months
Results: 14 of 16 patients (87.5%) reported significant pain relief at follow-up.
Limitations:
- No control group
- Retrospective design
- Subjective outcome measures only
- Small sample size
2. Interstitial Cystitis Study (2024)
Study design: Pilot study Participants: 12 women (ages 39-76) with moderate to severe interstitial cystitis who had failed pentosan polysulfate treatment Intervention: Intravesical (bladder) injection of 10mg BPC-157 Follow-up: 6 weeks
Results: 10 of 12 patients reported complete resolution of symptoms. The remaining 2 experienced 80% symptom reduction. No adverse events reported.
“This is the first report of intravesical BPC-157 injection to help patients with moderate to severe interstitial cystitis.” — Lee et al., Alternative Therapies in Health and Medicine, 2024
Limitations:
- No control group
- Small sample size
- Short follow-up period
- Single-site study
3. Intravenous Safety Study (2025)
Study design: Pilot safety/pharmacokinetic study Participants: 2 healthy adults (one 58-year-old male, one 68-year-old female) Intervention: Day 1: 10mg IV infusion over 1 hour; Day 2: 20mg IV infusion over 1 hour Monitoring: Vital signs, ECG, comprehensive metabolic panel, thyroid function
Results: No adverse events. No clinically meaningful changes in any monitored parameters. Plasma concentrations returned to baseline within 24 hours.
“Intravenous infusion of up to 20 mg of BPC-157 in 2 healthy adults showed no adverse effects and was well-tolerated.” — Lee & Burgess, Alternative Therapies in Health and Medicine, 2025
Limitations:
- Only 2 participants
- Very short observation period
- No long-term follow-up
- No efficacy endpoints
What These Studies Tell Us—And What They Don’t
What We Can Reasonably Conclude
Short-term tolerance appears acceptable: Across all three studies (roughly 30 participants total), no adverse events were reported. This is encouraging, though the sample size is too small for definitive safety conclusions.
Various administration routes seem feasible: Intraarticular, intravesical, and intravenous administration were all tolerated without apparent issues.
Some therapeutic signals exist: The interstitial cystitis results in particular suggest potential efficacy, though this needs placebo-controlled confirmation.
What Remains Unknown
Long-term safety: The longest follow-up was 12 months for knee pain patients. We have no data on years of use.
Optimal dosing: Without proper pharmacokinetic studies, dosing recommendations remain theoretical.
Drug interactions: No human data exists on how BPC-157 interacts with medications.
Cancer risk: BPC-157 promotes angiogenesis (blood vessel formation). Whether this could theoretically support tumor growth in humans is unknown.
Efficacy for most claimed uses: Gut healing, tendon repair, nerve regeneration—none of these common use cases have human trial data.
Regulatory Status: Why This Matters
FDA Classification (2023)
In 2023, the FDA designated BPC-157 as a Category 2 bulk drug substance. This classification means:
- BPC-157 cannot be legally compounded by 503A or 503B pharmacies for human use
- The FDA identified concerns about immunogenicity (potential immune reactions)
- Peptide-related impurities in manufacturing pose risks
- Insufficient safety data exists to establish it’s safe for humans
The practical impact: any BPC-157 available in the US today comes from either overseas suppliers or domestic gray-market sources operating outside FDA oversight.
WADA Prohibition (2022)
The World Anti-Doping Agency added BPC-157 to the Prohibited List in 2022 under category S0: Non-Approved Substances. Key points:
- Banned at all times—in and out of competition
- No Therapeutic Use Exemptions are available
- Athletes risk disqualification for any detected presence
- Also appears on the DoD Prohibited Dietary Supplement Ingredients List
What “Not Approved” Really Means
BPC-157 is not approved for human therapeutic use by any regulatory agency in the world—not the FDA, EMA, or any other authority. This isn’t just a technicality. It means:
- No standardized manufacturing requirements exist
- No quality control oversight applies
- No batch-to-batch consistency is guaranteed
- Purity and actual content can vary wildly between sources
The Quality Control Problem
Beyond the limited clinical data, anyone using BPC-157 faces a practical challenge: product quality.
Manufacturing Concerns
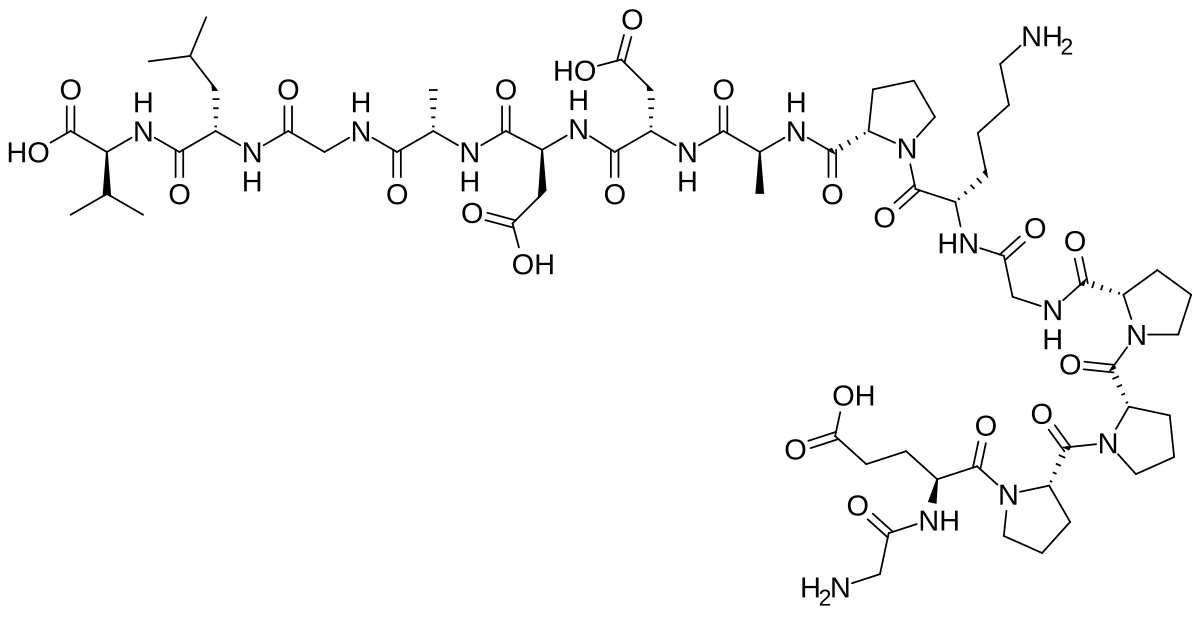
Peptides are complex molecules. Proper synthesis requires:
- Precise amino acid sequencing
- Accurate folding
- Removal of synthesis byproducts
- Sterile handling and packaging
Without regulatory oversight, there’s no guarantee any given BPC-157 product contains what the label claims.
What Testing Has Found
Independent analyses of peptides sold as “research chemicals” or “supplements” have found:
- Products containing different peptides than labeled
- Purity levels far below claimed percentages
- Bacterial contamination
- Heavy metal contamination
- Incorrect concentrations
This isn’t theoretical—it’s documented. When you use unregulated peptides, you’re trusting the manufacturer’s quality control without any third-party verification requirement.
Protecting Yourself
If you choose to use BPC-157 despite limited human data:
- Demand Certificates of Analysis (COAs) from third-party labs
- Verify the lab actually exists and conducted the testing
- Look for HPLC purity testing showing >98% purity
- Check for endotoxin testing (especially for injectables)
- Be skeptical of unusually low prices
Use our dosing calculator to ensure accurate reconstitution and dosing.
Comparing BPC-157 to Other Healing Peptides
BPC-157 isn’t the only regenerative peptide with research interest. Here’s how the human evidence compares:
| Peptide | Human Studies | FDA Status | Key Evidence Gap |
|---|---|---|---|
| BPC-157 | 3 pilot studies (~30 subjects) | Category 2 (cannot compound) | No RCTs, no pharmacokinetics |
| TB-500 | Even fewer | Not evaluated | Essentially no human data |
| GHK-Cu | Limited cosmetic studies | Allowed in topicals | Systemic use data lacking |
BPC-157 actually has more human data than most research peptides—which says more about the state of peptide research than about BPC-157’s evidence base.
What Would Proper Trials Look Like?
For BPC-157 to move from “experimental” to “evidence-based,” the research community would need:
Phase I (Safety)
- 50-100 healthy volunteers
- Multiple dose levels
- Comprehensive pharmacokinetic profiling
- Adverse event monitoring for 4-8 weeks minimum
Phase II (Efficacy Signals)
- 100-300 patients with specific conditions
- Randomized, placebo-controlled design
- Validated outcome measures
- 3-6 month follow-up minimum
Phase III (Confirmatory)
- 500-3000 patients
- Multi-site trials
- Long-term safety monitoring
- Comparison to existing treatments
Currently, we’re stuck before Phase I even completes. The cancelled 2015 trial set this research back nearly a decade.
The Anecdotal Evidence Question
Given limited clinical data, many BPC-157 users point to anecdotal reports as supporting evidence. Thousands of people claim benefits on forums, social media, and podcasts.
Why Anecdotes Are Unreliable
- Placebo effect: Expecting improvement creates real perceived improvement
- Selection bias: People who feel better are more likely to report
- Regression to the mean: Injuries often improve on their own
- Confounding variables: Diet, rest, other treatments
- No verification: Claims can’t be independently confirmed
Why Anecdotes Still Matter
Anecdotal reports aren’t worthless—they generate hypotheses worth testing. The consistent themes in BPC-157 reports (gut healing, tendon recovery, reduced inflammation) align with animal research and suggest real effects may exist.
But anecdotes can’t replace trials. They can tell us what to study, not what to conclude.
Making Informed Decisions
Given everything above, how should you think about BPC-157?
The Conservative Position
Wait for better evidence. The animal data is promising, but “promising animal data” describes countless compounds that failed in humans. The lack of safety pharmacokinetics is particularly concerning—we don’t actually know how humans metabolize this peptide.
The Risk-Tolerant Position
Some individuals accept the current evidence gaps given:
- Strong preclinical data
- Favorable (if limited) pilot study results
- Absence of reported serious adverse events
- Personal risk-benefit calculations
Questions to Ask Yourself
- What am I trying to treat? Is there an evidence-based alternative?
- What’s my risk tolerance? Are you comfortable with unknown unknowns?
- Can I source quality product? Do you have access to verified, tested peptides?
- What’s my exit strategy? How will you monitor for problems?
- Have I consulted a healthcare provider? Particularly important if you have existing conditions
Frequently Asked Questions
Are there any BPC-157 human trials currently recruiting?
As of December 2025, no registered clinical trials for BPC-157 are actively recruiting on ClinicalTrials.gov. The research appears to be at a standstill following the cancelled 2015 Phase I study.
Why did the Phase I trial get cancelled?
No public explanation was provided. Possible reasons include funding issues, regulatory concerns, or preliminary data that didn’t support continuation. Without official disclosure, we can only speculate.
Is the lack of adverse events in human studies meaningful?
It’s encouraging but not conclusive. With fewer than 30 total subjects studied, rare adverse events wouldn’t be detected. Proper safety assessment requires larger sample sizes and longer observation periods.
Could BPC-157 ever become FDA-approved?
In theory, yes. In practice, it would require a pharmaceutical company to invest tens of millions in clinical trials. The lack of patent protection (BPC-157 is a naturally-derived sequence) makes this investment unattractive commercially.
Is it safe to use BPC-157 while taking other medications?
Unknown. No drug interaction studies have been conducted in humans. If you take medications—particularly those affecting blood pressure, clotting, or immune function—discuss with a healthcare provider.
The Bottom Line
BPC-157 represents a frustrating gap between promise and proof. The animal research is extensive and consistent. The mechanistic rationale is sound. Early human signals are positive.
But we’re still waiting for the kind of evidence that distinguishes proven therapies from experimental compounds.
What we know:
- BPC-157 shows remarkable effects in animal models
- Three small human studies report positive results and no adverse events
- Short-term tolerance appears acceptable based on limited data
What we don’t know:
- Long-term safety in humans
- Optimal dosing for various conditions
- Drug interactions
- Efficacy for most claimed uses in humans
- Whether animal benefits translate to people
The regulatory reality:
- FDA has restricted compounding due to safety concerns
- WADA prohibits use by athletes
- No country has approved BPC-157 for therapeutic use
If you choose to use BPC-157, do so with clear eyes about the evidence gaps. Source carefully, dose conservatively, and monitor closely. And hope that someday, proper trials will finally answer the questions that decades of animal research have raised.